In the words of the National Neurological Disorders and Stroke, a stroke is a brain attack. What makes stroke terrifying is how quickly it permanently damages the brain when oxygen is no longer supplied to support brain function, making time an incredibly rare resource in these circumstances. To save time in the treatment of a stroke, a new telemedicine approach to stroke treatment, called telestroke medicine, is one of the most successful implementations of telemedicine that helps administer emergency treatment to patients just in time. In this article, we will give an overview of how telestroke medicine operates and discuss some of its advantages and implementations.
What is Telestroke Medicine and How Does It Work?

Mayo Clinic defines telestroke medicine, or stroke telemedicine, as treating stroke from a distant location. The patient at the originating site will be treated by stroke specialists from a distant site through the use of telecommunication equipment such as high-resolution telehealth cameras, medical monitors, internet and digital imaging communication systems, teleconferencing software, smartphones/tablets, and sometimes even through robotic telepresence. This allows the stroke specialists from the distant site to observe the real-time state of the patient to make accurate assessments and diagnoses.
This outlines the basic procedures of telestroke medicine:
- Diagnostic/Neurological Examinations: The health practitioners on the originating site often start with imaging and diagnostic tests through telehealth cameras that track eye movement
and digital imaging like CT scans to enable the stroke team on the distant site to identify the type of stroke, determine the best treatment approach, and provide guidance to the health practitioners via a teleconferencing session. The specialist team often consists of neurologists, radiologists, and possibly neurosurgeons, all of whom offer their expertise in the case of a stroke occurring.
- Administration of Treatment: If the originating site has the proper personnel and equipment to administer treatment, treatment can begin immediately. Ischemic stroke is often treated with thrombolytic therapy if a stroke patient arrives within the 4.5-hour treatment window. Decisions about further interventions, like mechanical thrombectomy, are also made at this time. In the case of hemorrhagic stroke, reducing bleeding in the brain is of utmost importance, sometimes even requiring surgery.
- Continued Monitoring, Care, and Rehabilitation: Continuous monitoring of the patient is then conducted in a stroke unit or ICU, so health practitioners can continuously care for the patient and conduct patient monitoring remotely and rehabilitation planning. After treatment can be conducted through telerehabilitation, making rehabilitation more accessible.
Advantages of Telestroke Medicine
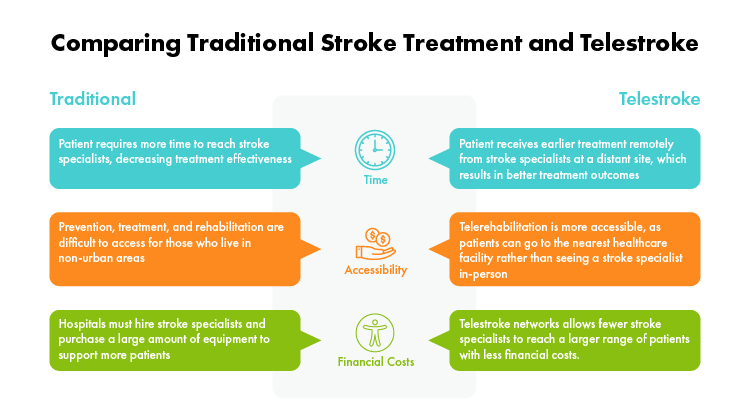
Why should healthcare practitioners integrate telestroke medicine into their stroke treatment? The most convincing reasons are to save time and increase patient accessibility to stroke prevention, treatment, and rehabilitation.
- Reduction of Time to Receiving Treatment:
Undoubtedly, the biggest difference between Telestroke Medicine and Traditional Stroke Treatment is the time in which it can start. Telestroke medicine can begin much earlier than traditional stroke treatments, substantially reducing the risk of mortality and resulting in better patient outcomes due to faster intervention.
- Increased Accessibility to Prevention, Treatment, and Rehabilitation:
People who live in non-urban areas — such as seniors, rural residents, indigenous people, or low-income individuals — have a harder time traveling longer distances to receive stroke treatment. With telestroke medicine, these groups gain more access to stroke specialists. Stroke prevention and telerehabilitation are also simpler for patients, as they can access it at a location closer to home or even access from home.
- Reduce Costs:
Since in-patient treatment and rehabilitation are extremely costly, hospitals can take advantage of telestroke networks, which according to research can help hospitals save over US$350,000 per year and US$2,227 per patient in nursing home costs.
Embracing Telestroke Medicine — A Prime Model of Effective Telehealth
Telestroke medicine emerges as a transformative force in stroke treatment, bridging the gap between patients and specialized care regardless of geographical constraints. By leveraging technology to assist with diagnosis and intervention, telestroke not only saves crucial time but also extends the reach of stroke specialists to communities previously underserved.
Applications of Telestroke Medicine
Rural Telestroke Care
Telestroke medicine differing from traditional stroke treatment uses technologies and communication tools to involve specialists from a distant site to help diagnose and treat local patients with VTE problems or stroke. After emergency procedures are implemented on the patient, telestroke medicine in the rural setting starts upon the patient’s arrival at the originating site, often a small rural health facility such as critical access hospitals (CAH) in the US. The originating site connects with the distant site, generally a larger urban hospital such as tertiary hospitals with stroke centers. The neurological specialists in the distant site will instruct the healthcare practitioners in the originating site on diagnosis and treatment. They may share clinical protocols from their hospital and cooperate to develop systems customized for their rural facility.
Advantages
- No need to hire in-house specialist: In typical stroke care, a hospital needs to have an in-house neurology specialist. With telestroke medicine, the rural hospital does not have to afford an in-house neurology specialist while enjoying the benefits of having one.
- Better Allocation of Resources: The rural hospital can utilize their limited resources on the equipment that reaps the greatest benefits such as essential medical equipment utilized the most (such as digital imaging and communication systems, smartphones, and tablets) and telemedicine equipment (such as medical-grade telehealth cameras and software or telehealth carts) for more advanced and specialized treatment.
- Minimal Waiting Time and Transfer Time: When truly impossible for the rural health facility to handle alone, a patient can be transferred safely with the instruction and supervision of the remote specialist to a larger hospital when necessary. This minimizes the time the patient is waiting and unsupervised and helps drastically improve chances of recovery for stroke patients.
Urban Telestroke Care
While telestroke care is most commonly applied in the rural setting, the large urban hospital can also utilize the telestroke medicine setup for better treatment results, the earlier the better: such as on the ambulance. In this case, the originating site would be where the patient and emergency medics are and the distant site would be the large urban hospital.
If an urban hospital established a mobile stroke unit in the ambulance, it would be possible to administer higher quality treatment earlier rather than just maintaining and monitoring a patient’s vitals. The distant site neurological specialists can instruct the emergency medics in the originating site on diagnosis and treatment.
If a hospital established a telestroke medicine setup between the urgent care center and the neurologist, then higher quality treatment again can be administered at an earlier time, leading to better treatment results.
Advantages
- Earliest treatment time possible: stroke-specific treatment can begin once emergency medics arrive where the patient is located. Time of treatment is one of the crucial indicators of how well a patient will recover after a stroke.
Embracing Telestroke Medicine — A Prime Model of Effective Telehealth
Telestroke medicine emerges as a transformative force in stroke treatment, bridging the gap between patients and specialized care regardless of geographical constraints. By leveraging technology to assist with diagnosis and intervention, telestroke not only saves crucial time but also extends the reach of stroke specialists to communities previously underserved while saving precious time for treatment.
Explore how AVer’s Connected Health Solutions offer a win-win for everyone involved and the future of Telestroke Medicine.
References